Download the Defibrillator Patient Information Sheet
 A defibrillator (also called “ICD”) is a device that is used to treat patients who are at risk for dangerous rapid heart racing known as ventricular tachycardia (VT) or ventricular fibrillation (VF).
A defibrillator (also called “ICD”) is a device that is used to treat patients who are at risk for dangerous rapid heart racing known as ventricular tachycardia (VT) or ventricular fibrillation (VF).
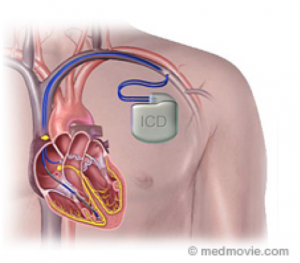
Defibrillators are made up of a generator (battery) and one or more leads (wires). The generator contains the baFery and computer circuits. Lead/s may be placed in the upper or lower chamber of your heart or in both places. The :p of the lead is placed against the inside wall of your heart and the other end connected to the generator. This allows the generator to send small electrical impulses to pace the heart or large electrical shocks to stop dangerous heart racing attacks.
The defibrillator implant procedure is performed at the hospital. In preparation for the operation, you will be given basic instructions by hospital staff. You will be asked not to eat or drink anything the morning of the operation. Someone else should drive you to the hospital and take you home Afterwards. If you are taking medications, it is usual prac:ce to omit the pills the morning of the operation. After you arrive at the hospital, everything will be checked in preparation for the operation. The staff will insert an intravenous drip. The use of conscious sedation or general anesthesia will be decided on a case-by-case basis. You will be given an:bio:cs prior to the procedure. Local anesthetic (similar to “dental freezing”) will be injected into the skin typically under the left collar bone. A small incision will be made in this area and the wire/s will be inserted into the vein, and advanced into the heart chamber. The wire/s are moved to the right position under x-ray guidance and secured in place. The wire/s are connected to a generator. Testing is performed to ensure sa:sfactory function of the defibrillator. The wound is then closed. A transparent water-proof dressing and a pressure dressing are applied over the wound.
You will monitored on the ward overnight and antibiotics will be given. A chest x-ray will be routinely performed to document the position of the leads and to exclude any injury to the lung. You will be discharged the next morning if all the checks are satisfactory. You will be given oral antibiotics for 1-2 weeks. You should not drive for at least 2 weeks, and avoid lifting the arm on the same side as the device above shoulder height for 6 weeks. You should leave the pressure dressing for 2 days. After that you can shower with the transparent dressing. The transparent dressing can be removed by your GP After 7 days. There are usually no stitches to remove. It is common to experience a mild ache over the area for 2-3 weeks and over-the counter pain killers may be required. It is also usual to notice some bruising over the site which will move down your left arm and chest. This should resolve After a few weeks. Please see your GP and ask him/her to contact Dr Sy immediately if you develop any of the following:
As in any medical procedure, you should be aware of potential risks. The overall risk of a complication is only 1-2%. The risks are:
Q. How long will my defibrillator last? A. On the average, 6-8 years
Q. How often does it need to be checked? A. After 3-4 weeks. Then every 6 months.
Q. What do I do if I get a shock? A. You will be provided with advice and a contact number to ring if you experience a shock from the device. If you experience 2 or more shocks in a single day, you should present to the nearest emergency department.
Q. I am on blood thinners. Does that matter? A. Yes. Please let us know! Dr Sy will advise management of your blood thinners around the time of your procedure.
Other resources www.hrsonline.org (Heart rhythm society)